Knee Menisci – understanding the anatomy, biochemistry, and bio-mechanics is crucial for clinical interpretation and management.
INTRODUCTION
The menisci are two discernible crescent-shaped fibro-cartilaginous structures that are found between the femoral and tibial condyles. Although they were considered to be the functionless remains of leg muscles for many years, the menisci are now well defined as the important component of the functional anatomy and complex biomechanics of the knee joint.1 The unique shape, composition, mechanical properties, anatomical entheses and insertional ligaments of menisci have made menisci the proper structure for load transmission, shock absorption, joint stability and congruency, joint lubrication, proprioception and joint nutrition in the knee joint.1-3 This growing knowledge on physiological and functional importance of menisci has changed the therapeutic approach to meniscal injuries and diseases towards the repair and rehabilitation rather than the removal of meniscus.3
Load transmission being the primary function of menisci, any changes in menisci due to injury, disease or aging may produce significant changes in the knee joint biomechanics and hence in the load transmission mechanism. It is crucial to understand the anatomy, biochemistry, and biomechanics of the meniscus to clinically interpret the meniscal injuries or disorders and predict the healing or rehabilitative paradigm thereby determining the concrete clinical or therapeutic approach of treatment.
LITERATURE REVIEW
Anatomy
Embryology
Menisci are formed from a condensation of an intermediate layer of mesenchymal tissue and develop as a highly vascular and cellular distinct structure between the 8th and 10th week of fetal development. 1,3,4 The studies have shown consent that increased joint motion and weight bearing cause the histological changes in menisci; cellularity decreases while increase in collagen content and blood supply retract and limit to the periphery.1,5
Functional anatomy
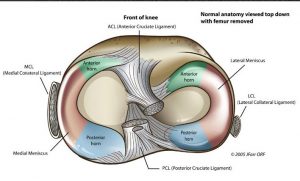
Although menisci are distinct structure, functionally they are considered as the extension of the tibial plateau to increase the tibial articular surface and its relative depth. The proximal concave meniscal surface articulates with femoral condyles while distal flat surface articulates with convex tibial condyle laterally and concave tibial condyle medially forming a meniscotibial socket which contributes to the stability of knee joint and load transmission by converting into hoop stresses.1,6 The firm anatomical entheses of anterior and posterior horns of menisci to bone via insertional ligaments are crucial for the load distribution and is considered to be the part of entire functional unit of menisci.3,4
Medial Meniscus (MM)
The semilunar or C-shaped normal MM has a larger anteroposterior length (3.5-5cm) than its transverse width (2.5-3cm).1,2,7,8 Although the studies have shown minimum variations in the height and width of anterior horn, mid-body and posterior horn of the medial meniscus, they have a common finding that the MM is significantly wider in its posterior horn which progressively narrows as it approaches anterior horn.1,2,4,9 However, these studies have used different measurement techniques, cadaveric or surgical or in vivo measurements and measurement in different knee joint positions. Future studies should focus to provide standard measurement technique and criteria to define a normal meniscal size which contributes to diagnose variants in meniscus size such as discoid or large MM and provides support during treatment, rehabilitation or surgical replacement of meniscus. The recent in vivo MRI finding of 174 normal menisci by Erbaci et al9 has shown the results in accordance with the range of measurements shown by other studies mentioned above (Table 1).
The compression force generated by a load between femur and tibia tends to push wedge-shaped MM outwardly in a radial vector.10 This displacement is resisted by firm anatomical entheses of the anterior horn (AH) and posterior horn (AH) of meniscus generating the ‘hoop stresses’.6 Insertional ligament of AH is attached as a band in the area of intercondylar fossa of tibia about 6 or 7 mm anterior to the attachment of anterior cruciate ligament (ACL) and posterior horn is attached to the tibial intercondylar fossa between the posterior attachment of lateral meniscus (LM) and posterior cruciate ligament (PCL).
| N.174 | Lateral meniscus | Medial meniscus | P-value | |
|
Anterior Horn |
SH | 4.33±0.98 | 5.32±0.95 | <0.001 |
| CW | 8.88±2.3 | 7.78±1.86 | <0.001 | |
|
Mid body |
CH | 4.94±0.99 | 5.03±0.91 | NS |
| CW | 8.37±0.83 | 7.37±2.65 | <0.001 | |
|
Posterior horn |
SH | 5.36±1.03 | 5.53±0.99 | NS |
| CW | 9.70±1.69 | 11.71±2.63 | <0.001 |
Table 1: Dimensions of the knee menisci (mm). SH sagittal height; CW coronal width; CH coronal height; NS non significant. (From Erbaci et al. 2004).
However, studies have shown the variants in anterior horn attachment of medial meniscus (AHMM). Out of 953 knees, arthroscopic study done by Ohkoshi et al11 found 98 cases of variant AHMM which they classified as: ACL type, where AH attached to ACL; Transverse ligament type, where AH attached to transverse ligament; coronary ligament type, where AH attached to coronary ligament and infrapatellar type where AH attached to infrapatellar synovial fluid. This result was in support of the 22.6% of variant AHMM cases reported by Ikeuchi12. Kohn et al7 reported 64% of cases with transverse ligament type variant in AHMM in their study of 46 cadaveric knees. Both Ikeuchi12 and Ohkoshi11 studies were done in Japanese population only. However these studies have shown interesting clinical and pathological significance of these variants.
Out of 93 knees with variant AHMM, Ohkoshi11 have demonstrated ACL rupture in 19 knees (18.4%), isolated medial meniscal tear in 23 (22.3%), patellar lesions in 13 knee (10%) and 12 knees (11.7) with diagnosis of anterior knee pain syndrome. The author has opined the hypermobility of AH of MM as the primary cause behind these clinical manifestations which is backed by the recent study done on effect of anterior medial meniscus detachment on ACL tear by Holgado et al.13 Detail study about the incidence and clinical significance of variant AHMM is important and also the standard quantification of mobility of AH of MM is a big gap for further studies.
Blood supply and innervations
Only 10% to 30% of peripheral medial meniscus remain vascular and is supplied by superior and inferior branches of medial genicular arteries.2,4 The horns of meniscus are richly supplied by radial branches of perimeniscal capillary plexus and synovial vessels which are supplied by middle genicular artery.4 Early weight bearing as soon as possible is important during rehabilitation to keep meniscus intact as avascular regions of meniscus get nutrition supply by a mechanical pumping mechanism provided by intermittent compression of meniscus.4
A posterior articular nerve is the primary nerve supply to menisci however the part of the medial meniscus is innervated by the branches of medial articular nerve.3 Anatomical and clinical studies on the innervations of menisci are conflicting. Kennedy et al14 reported that meniscal innervations do not extend to meniscal body however demonstrated the presence of numerous axons, free nerve endings, specialized receptors like Golgi tendons ending in perimeniscal capsular tissue. Day et al15, however, reported the innervations into outer third of meniscus with rich innervations at the horns and suggested vasomotor function of medial innervations.
Zimny et al highlighted that neural elements may act as afferent transmitters and also proposed the protective and proprioceptive feedback mechanism from meniscal innervations. Concrete knowledge of these neural presentations and information is important as it suggests that menisci may play a vital role in knee joint proprioception and in afferent/efferent transmissions and thus affect clinical interpretations.
Meniscal functions and biomechanics
Biphasic nature of the meniscus (solid phase composed of collagen and other extracellular matrix and fluid phase consists of water and electrolytes) facilitates the primary functions of menisci; load transmission and shock absorption, joint stability, proprioception, lubrication and distribution of nutrition.4,17
Woo et al17 demonstrated that up to 50% and 85% of axial loads are transmitted through menisci with a knee at full extension and 900 flexions respectively. This may describe the clinical application of menisci that meniscal tears, partial and total meniscectomy or degeneration are always associated with degeneration or calcification of cartilage, osteoarthritis and bone remodeling.
Dynamic meniscal motion during joint movement maintains the optimal load bearing efficiency, shock absorption, and joint congruency. Thomson et al18 reported 5.1mm and 11.2mm of posterior excursion of medial and lateral meniscus respectively during full flexion from the full extension. This study, however, may not represent in a vivo weight bearing situation as it was studied in unloaded cadaver knees. Vedi et al19 later observed in vivo, and found lesser posterior excursion; 3.9/3.8 mm and 5.6/4.0 in weight bearing/non-weight bearing conditions of medial and lateral meniscus respectively (Fig. 1). However both the studies reported posterior excursion of meniscus during flexion and that anterior horn are more mobile than posterior.

Fig. 1: The mean movement (mm) in each meniscus from an extension (shaded) to flexion (hashed) in (a) the weight bearing and (b) the unloaded knee. (From McDermott et al. 2010).
Medial Meniscal tears
Medial meniscus posterior root tear (MMPRT) is the most common meniscal tear and is an important risk factor for the development of osteoarthritis.3 Despite this common pathology and clinical importance, very few studies have been done to identify the common risks factors to meniscal tears. Ozkoc et al20 have reported old age, high BMI and oriental lifestyle with use of lotus position and squatting as the primary risk factors for MMPRT. But they have not provided any particular data or mechanism of injury to support their report.
Bin et al21 performed kinematic analysis of medial meniscus and supported Ozkoc20 that impingement of posterior meniscal segment is common during dynamic movement of meniscus resulting in degeneration and hence prone to tear. However, Hwang et al22 reported no association between age and lifestyle and meniscal tears but demonstrated higher BMI, varus mechanical axis angle and lower sports activity level as major risk factors for meniscal tears. There is strong association between degenerative joint disorders and medial meniscus extrusion which ultimately can provoke meniscal tear.23
All these studies have just focused on degenerative meniscal tears; however, trauma is one of the most common causes of meniscal tears and is commonly associated with ACL tears.24 23 out of 98 knees with variant AHMM studied by Ohkoshi et al11 have shown medial meniscus tear with no history of trauma. Future studies must effort to identify the major risk factors and possible mechanism of meniscal injuries which is clinically important to prevent common disorders like osteoarthritis and ACL tears.
Reference

One Comment