Perspective: Efficacy of spinal manipulative therapy in the treatment of symptomatic lumbar disc herniation
Efficacy and safety of spinal manipulation therapy (SMT) in the treatment of symptomatic lumbar disc herniation (LDH) is the focus of this essay. In cases of LDH, high-velocity low amplitude, short lever rotational technique in side-lying posture is the commonly practiced technique. This perspective discusses on four different essential and practical considerations of spinal manipulation therapy in the treatment of LDH; inclusion/exclusion criteria, clinical efficacy, mechanism of action, and risk/benefit and safety.
Background:
Sciatica secondary to lumbar disc herniation is one of the common causes of low back pain with radiating pain in the leg with estimated lifetime incidence of between 2% and 40%. It is also a major source of disability resulting in to functional impairments[14, 21]. Many studies[17,21,26] have shown consensus over a trial of conservative or non-operative treatment prior to surgical intervention for majority patients with symptomatic LDH unless immediate surgery is indicated for cauda equina syndrome (CES) or rapid and progressive neurological deficits. However, conclusive evidence for the efficacy of both conservative and surgical approaches in the treatment of symptomatic LDH is yet to be determined and Spinal Manipulation Therapy is no exception [22].
Many kinds of literature have advocated safe use of SMT and its clinical efficacy[7,8,14,16,21,22] whilst some authors are against the use of spinal manipulation therapy and have demonstrated various complications of SMT in cases of LDH[2,17,19]. This article aims to discuss evidence published on various literature on risks and benefits, a possible mechanism of action, and its clinical implications, and efficacy of side lying rotational high-velocity low-amplitude thrust (HVLAT) manipulation of the lumbar spine in the management of patients with symptomatic LDH like sciatica due to LDH. This study, therefore, may support the development of evidence-based standard clinical guidelines to practice spinal manipulation therapy in cases of LDH.
Discussion:
Inclusion/exclusion criteria:
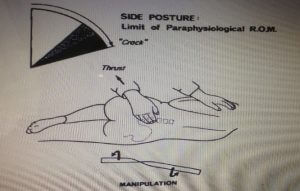
Various forms of spinal manipulation techniques are practiced in the treatment of low back pain. However, high-velocity low amplitude, short lever rotational technique in side-lying posture (Fig. 1) is the common technique being practiced in cases of LDH [4,14,18]. Absolute indications and contraindications of spinal manipulation therapy in LDH is another complex aspect of debating. However, most of the studies [14,21,22] have reported CES and rapidly progressing neurological symptoms as absolute contraindications for spinal manipulation therapy. Many reports have discussed and highlighted the importance of proper case history and physical examination before making a decision on SMT intervention [14,21]. Some of the common exclusion criteria for SMT reported in the literature are listed in table 1.
Table 1.
|
|
|
Table 1: Exclusion criteria for Spinal manipulation therapy.
Reference: McMorland et al (2010); Santilli et al (2006).
Clinical efficacy:
Various forms of studies like case series, prospective studies, literature reviews, randomized controlled trials (RCTs) have concluded and highlighted the clinical efficacy of spinal manipulation therapy in LDH. However, due to methodological weaknesses, most of the studies are unreliable to develop as a strong basis to make a clinical decision [22]. Burton &Tillotson (2000) performed a comparative analysis of the efficacy of SMT and chemonucleolysis in symptomatic LDH and reported significant improvements in back pain and disability scores initially at two and six-week periods following SMT in comparison to chemonucleolysis. This study could not define long-term effects of spinal manipulation therapy. Also, inclusion of soft tissue stretching, low amplitude passive
Burton &Tillotson (2000) performed a comparative analysis of the efficacy of SMT and chemonucleolysis in symptomatic LDH and reported significant improvements in back pain and disability scores initially at two and six-week periods following SMT in comparison to chemonucleolysis. This study could not define long-term effects of spinal manipulation therapy. Also, inclusion of soft tissue stretching, low amplitude passive articular maneuvers and a small number (n=40) of participants are other major drawbacks of the study. However, due to overall crude cost saving, significant short-term efficacy and no evidence of complications following manipulation; authors concluded SMT as considerably safe and effective treatment option for patients with radicular symptoms like sciatica due to LDH.
SMT or surgery?
A prospective randomized clinical study done by McMorland et al (2010) is a well-designed and controlled study comparing the clinical efficacy of SMT against microdiscectomy in symptomatic LDH. This study demonstrated the same degree of improvement with SMT as shown by surgical intervention with 60% of success rate. This study also shows the fact that 40% of patient with an unsatisfied result from SMT improved significantly after subsequent surgical intervention whilst 15% of patients who failed surgical treatment failed to gain any further improvement with subsequent SMT. Despite the small sample size (n=40) in this study, stronger statistical techniques, intent to treat analysis and use of standard tools like McGill Pain Questionnaire, Roland-Morris Disability index and Aberdeen Back Pain Scale to assess quality of life have adequately powered the demonstrated results to be clinically significant and suggested consideration of SMT prior to surgery in patients with symptomatic LDH.
Mechanism of action of SMT:
There is a lack of clear explanation of the conclusive mechanisms of action of spinal manipulation on outcome in symptomatic LDH. Several studies [13]have hypothesized reduction in intervertebral or intradiscal pressure at the end of thrust in spinal manipulation therapy. This hypothesis is also backed by a laboratory observation [1] on pressure peaks generated by sustained or abnormal loading of a disc which demonstrated that pressure peaks may be reduced by diminished intradiscal pressure induced by SMT. Earlier, a study [11] suggested that rotational movement and thrust during SMT may correct possible derangement of facet joints or subluxation of posterior elements near protruded disc, thereby releasing pressure or entrapment of nerve root and hence producing remarkable pain relief.
Similarly, researchers have discussed the reduction of paraspinal muscle spasm due to diminished H-reflex or by reflex contraction of back muscles caused due to stretching by high-velocity direct thrust [3,15]. Whilst some studies [24] suggested a direct effect of spinal manipulation therapy in activation of diffuse descending pain inhibitory system due to sudden stretching of ligaments, disc, joint capsule or muscles. However, all of these mechanisms of actions of spinal manipulation therapy are yet to be conclusively explained with strong evidence by conducting large standard RCTs to define strong clinical guidelines.
Risk/benefit and safety:
“The clinical efficacy of a treatment approach always needs to be balanced with the potential harm” [22]. A number of studies have reported various complications following SMT. Rivett et al (1997) reported several incidences of serious complications arising from spinal manipulation therapy in New Zealand. This retrospective study is based on the questionnaires posted to neurologists, neurosurgeons, orthopedic and vascular surgeons, which weakens the data in order to be determined as possible complications or adverse effects of SMT. Also, many cases that showed complications after manipulation described in this study were also found to be presented with underlying pathologies such as undiagnosed malignancies, VBI, and osteomyelitis which might have predisposed severe adverse response to manipulation therapy. However, this study warns and spotlighted the need of systemic and thorough clinical examination to screen contraindications prior to manipulative interventions.
A systemic review and risk assessment were done on the safety of spinal manipulation therapy in the treatment of LDH [16] have reported the risk of CES, worsened LDH and/or other complications in less than 1 in 3.7 million manipulations. This report stimulates the safe use of SMT in LDH when we compare with the published reports of complications of 1.5% to 12% with LDH surgeries [9,16] and 1% to 4% of NSAIDs users [5]. However, standard larger prospective study to determine the outcome and complications of SMT in LDH and its comparison with natural history or other treatment is still a big gap to fill in the manipulative therapy field. Meanwhile, according to Oliphant (2004) “neither NSAIDs nor surgeries have been proven to be more effective in the treatment of LDH than SMT”.
From biomechanic point of view
From a biomechanical perspective, a standard side lying rotational lumbar spinal manipulation at particular spine level does not involve any of the combination of compression, lateral bending and forward bending movements; the only loading condition known to cause posterior disc prolapse [8]. Also, some studies [1,8,18] have reported that torsional stresses produced during HVLAT spinal manipulation are not strong enough to generate adequate torque to rupture disc. Brinckman& Porter (1994) sliced annular fibers from anterior to posterior leaving only 1mm of annulus intact and then compression and flexion load is applied. Interestingly, only small bulge of 0.8mm of a disc was prolapsed whereas the significant size of disc protruded out through a complete annular tear with only a small compression and flexion load when only the small fragmented size of a disc as seen after discectomy was inserted.
Thus, already fragmented disc and fissured annular fiber by any reason may suggest the greatest risk factor for disc prolapse and hence must be considered and screened carefully prior to SMT intervention.
Summary
In conclusion, there is a lack of strong scientific evidence rather than negative evidence on the clinical efficacy of side lying rotational spinal manipulation in LDH. Reports have clearly demonstrated significantly minimal risks or complications of manipulation as a treatment for LDH compared to complications reported of the use of NSAIDs and surgeries. Therefore, spinal manipulations in LDH appear to be safe when used by appropriately trained practitioners based on detailed physical examination and careful screening of exclusion factors. It is always safe and reasonable to explain patients about potential risks and benefits of spinal manipulation therapy and take written consent, for the protection of both patients and therapists.
However, there is a clear indication for more well-designed larger prospective studies or RCTs to conclusively explain the mechanism of action of SMT, to determine strong clinical decision rules and clinical guidelines for spinal manipulation intervention in symptomatic lumbar disc herniation.
Reference
Download as PDFRelated Posts

Sports Rehabilitation. Study on Counter Movement Jump Performance in a Force Platform.

Sports Rehabilitation. The role of the biomechanist and physiotherapist as a team for athletes’ wellbeing and performance.

Hi There! We are searching for experienced people that might be interested in from working their home on a full-time basis. If you want to earn $500 a day, and you don’t mind writing some short opinions up, this is the perfect opportunity for you! Simply click the link here NOW!
Very good written story. It will be beneficial to anybody who usess it, including myself. Keep up the good work – can’r wait to read more posts.
Thankyou. Pls subscribe for new updates.
That is a really good tip especially to those fresh to the blogosphere.
Simple but very accurate information…
Appreciate your sharing this one. A must read article!