Shin Splints

What is Shin Splint?
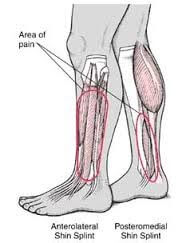
Shin splint is an overuse injury or repetitive injury of shinbone (tibia) area causing posteromedial or anterolateral shin pain.
Anterior tibial stress syndrome/anterior tibial periostitis/anterolateral shin splint
Musculotendinous overuse of tibialis anterior and extensor hallucis longus.
Anterolateral pain, pain on palpation of lateral tibia and anterior compartment.
Medial tibial stress syndrome/ medial tibial periostitis/posteromedial shin splint
Overuse injury resulting in periosteal inflammation of muscular attachments.

Muscles involved; tibialis posterior and medial soleus.
Most common with distal – posteromedial pain.
Etiology/risk factors
o Mainly due to stretch or overload periostitis of tibialis anterior, extensor hallucis longus, tibialis posterior, or medial soleus.
o Common in running, jumping activities on hard or uneven surfaces; more common with bad running shoes.
o Following sudden increase in training intensity, frequency, and duration (training mistakes)
(Tibialis anterior muscle must work hard in order to control the landing of the forefoot with each stride and also to maintain ankle dorsiflexion. Furthermore, running downhill demands more work of this muscle to prevent forefoot from slapping down)
o Muscle imbalance due to tight calf muscles.
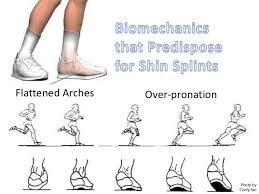
o Abnormal biomechanical alignment
(Pronation of foot/ flat foot – with flat foot tibialis posterior muscle gets stretched causing repetitive stress on its attachment in tibia leading to damage, inflammation and eventually becomes painful).
History of previous lower extremity injuries and hence compromising biomechanical alignment.
Clinical presentation of shin splints
–Vague, dull and diffuse pain along middle-distal third of length of posteromedial tibia (usually 4-12 cm proximal to medial malleolus)
–Pain at the start of exercise or running which decrease during exercises and return with rest (early stage). However, at chronic stage pain can be present all the time.
–Morning pain because of tissue stretching after long rest.
–Limited ROM. Stretching increase pain.
Examination
–Usually bilateral involvement
–Mild inflammation at painful area
—Pes planus/pronation of foot
–abnormal biomechanical alignment; knee (genu valgus or varus), tibial torsion, hip anteversion, sacroiliac joint, ankle or subtalar joint malalignment.
–muscle imbalances; tight calf muscles, weak core and hip muscles, weak or tight hamstring and quadriceps.
–Provocation test: pain on resisted dorsiflexion
Differential diagnosis
-Tibial or fibular stress fracture: Pain with running, point tenderness over fracture site, markable black line on lateral x-ray, night pain, reduced pain in morning, normal ROM
-Exertional compartment syndrome: severe cramping, diffuse pain, and tightness, symptoms begin 10min into exercise and resolve 30min after exercise, sensory or motor loss, elevated anterior compartment pressures, muscle weakness, limited ROM in an acute phase.
-Achilles, peroneal or tibialis tendinopathies.
-Sural nerve entrapment which presents symptoms in a dermatomal distribution.
-Lumbar radiculopathies which are radiating pain and increases mainly with flexion activities like sitting.
-Vascular disorders like popliteal artery entrapment, DVT, intermittent claudication.
-Tumors – often night pain, deep, nagging with some radiation.
-Anterolateral ankle impingement
Physiotherapy management
Acute phase
o Rest (2-6 weeks), ice, compression, taping
o To reduce inflammation; Iontophoresis, ultrasound, soft tissue massage
o Gentle stretching of the calf and tibialis muscles in order to improve flexibility and circulation.
Subacute phase
o Activity modification
–decrease running distance, duration, frequency, and intensity to comfort so as to exercise in pain-free level.
–avoid or reduce running uphill, downhill, uneven or hard surfaces in order to reduce stress and allow enough time to heal.
o Exercise program modification
–increase warm-up periods before exercise
–dynamic stretching and eccentric strengthening exercises of gastro-soleus muscles in order to maintain muscle balance.
–use of cross training regimen with low impact exercises so as to reduce stress or load impact on musculotendinous units.
–strengthening of core, abdominal, hip, thigh and leg muscles especially foot invertors.
–proprioceptive balance training in order to improve weight distribution among muscle groups.
o Biomechanical considerations
–manual therapy in order to correct any biomechanical abnormalities of the spine, sacroiliac, hip, knee or ankle joints and various muscle imbalances.
–use of foot support or orthotics especially in pes planus so that arches of the foot are improved or maintained.
–shoe modifications in order to maintain biomechanical alignment as well as to provide enough shock absorption.


I am only commenting to make you understand what a terrific encounter my cousin’s girl experienced using your web page. She realized numerous details, which include what it is like to possess a marvelous giving mood to let the others effortlessly learn a number of extremely tough subject matter. You undoubtedly exceeded people’s desires. Thanks for distributing these essential, trustworthy, revealing and as well as unique guidance on this topic to Tanya.